CRM helps, but healthcare AI needs context, compliance, collaboration and continuous learning to transform patient care.
When I began leading digital health programs over a decade ago, CRM was the shiny object. We believed that by implementing a unified platform, we could orchestrate seamless patient engagement, automate case management and bring intelligence into interactions that were otherwise siloed and manual.
But over the years and through multiple large-scale deployments across Fortune 10 healthcare organizations and life sciences clients, I have come to realize a tough truth: CRM is only one piece of the puzzle. In today’s healthcare environment, especially when scaling AI-driven capabilities, CRM needs to be part of a broader ecosystem that includes data architecture, compliance governance and contextual intelligence.
In this article, I will share how we evolved beyond CRM-first thinking, what CIOs should consider before scaling AI in regulated environments, and the foundational elements that truly drive transformation — not just implementation.
The limits of CRM in a healthcare setting
Healthcare is fundamentally different from other industries in terms of customer engagement. “Customer experience” in healthcare often includes life-altering decisions, sensitive health data and coordination across clinical, financial and operational systems. CRM platforms, while powerful, often don’t understand this context natively. As HIT Consultant notes, traditional CRM platforms often lack the adaptability needed for healthcare environments, where real-time clinical context and patient-specific nuances are essential.
In one of my earlier roles, we implemented a CRM system to support patient onboarding for specialty therapies. The initial goal was simple: streamline intake and automate status tracking across insurance, benefits verification and care coordination. Technically, it worked. But practically, we found ourselves hitting limitations quickly:
- The CRM system lacked access to longitudinal patient data, stored across legacy EHRs and third-party vendors.
- Workflow rules were based on static logic and couldn’t adapt to dynamic patient journeys.
- Even with dashboards, frontline teams lacked insights to act proactively. We were still reacting to issues, not anticipating them.
In one specific instance, a CRM task automation system failed to escalate a stalled benefits case because the delay occurred outside the defined “case status” logic. A patient’s treatment was postponed by five days because no one was alerted, despite all the information being present across systems. That was a wake-up call.
We weren’t failing because of bad configuration or poor training. We were failing because the system was never designed to operate as a real-time decision engine. That’s when we started rethinking what “customer relationship management” should really mean in healthcare.
Where AI moves the needle
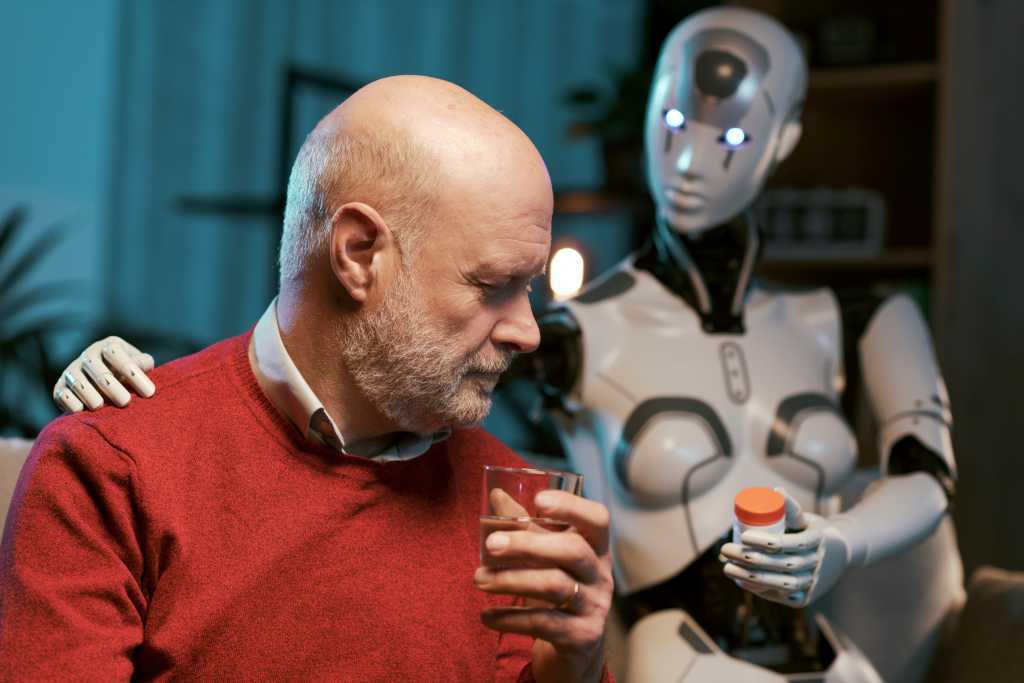
Adding AI to CRM isn’t just about plugging in predictive models or using chatbots. It’s about embedding intelligence at decision points that matter and doing it in a way that respects compliance, explainability and patient trust.
In a recent deployment, we introduced an AI layer on top of our CRM workflows. The goal was to help patient services reps prioritize cases that were at higher risk of disruption, not just those that were overdue. To do that, we had to go well beyond the CRM platform:
- We integrated external data sources, including social determinants of health (SDOH), prior claims activity and historical case-resolution times. The CDC defines social determinants of health (SDOH) as non-medical factors like housing, education and economic stability that deeply influence outcomes.
- We built a governance model in collaboration with legal and compliance teams to ensure decisions could be audited and explained.
- Most importantly, we invested in change management training for our case managers — not just on how to use the AI tool, but when to trust it and when to override it.
The results weren’t just technical wins; they changed how our teams worked. AI wasn’t replacing decision-making; it was augmenting it with context, speed and foresight.
For CIOs, this shift is critical. AI succeeds when it’s framed not as a replacement for CRM, but as a strategic layer that guides workflow, augments data and enhances human judgment.
A framework that works: 4 pillars for scaling AI beyond CRM
Through multiple transformation programs, I’ve come to rely on a simple but effective framework that helps ensure AI deployments scale beyond CRM functionality and deliver real outcomes. I call it the 4C model:
1. Context
Without a deep understanding of the patient journey, even the best AI models will fail. Context means integrating clinical, operational and behavioral data, not just CRM objects like cases and tasks. For example, if a predictive model only knows that a case is “open,” it can’t distinguish between a two-day delay and a systemic issue that could delay therapy for weeks. When we added claims and provider data, our models went from being descriptive to truly predictive.
Tip: Start with a journey map, not a data model. The best insights often emerge when you overlay the “lived” patient journey with the system-generated one.
2. Compliance
In healthcare, ethical AI is non-negotiable. You need to build explainability, traceability and fairness into your models, not as afterthoughts, but as core architectural components. As highlighted by the World Economic Forum, tech leaders like Microsoft are building responsible AI frameworks that prioritize ethics, human oversight and transparency. In one of our deployments, we ran fairness audits on our discontinuation models and discovered subtle skews by geography. Without those checks, the AI would have quietly amplified inequities. Addressing compliance up front ensured we could scale responsibly.
3. Collaboration
IT can’t do this alone. Some of our best AI outcomes came when compliance officers, frontline users and clinical leads co-designed workflows and challenged assumptions. In one case, a nurse navigator pointed out that the model’s recommendations conflicted with how providers structured patient follow-ups. By bringing her into the design process, we adjusted the algorithm and the workflow together, resulting in faster adoption and more trust in the system. Cross-functional teams are not optional — they’re mission-critical.
4. Continuous learning
Once deployed, AI must evolve. Monitor for model drift, feedback loops and unintended bias. Think of it as a digital organism, not a static tool. To support transparency and auditability, tools like Google’s What-If Tool allow teams to test how changes in input data affect predictions, helping to uncover potential bias before deployment. In practice, this means setting up monitoring dashboards, retraining cycles and governance reviews. On one project, we detected drift within six months as prescribing patterns shifted post-COVID. By retraining quickly, we avoided inaccurate prioritization that could have derailed trust in the system.
Advice to CIOs: It’s not just about tools, it’s about timing and trust
If you’re in a CIO or digital leadership role and planning to scale AI across patient engagement or healthcare operations, I’d offer the following guidance based on lessons I’ve learned (sometimes the hard way):
- Don’t start with tools, start with trust. Build governance models early, not after you go live.
- Don’t fall into the trap of deploying AI as a checkbox exercise. Choose opportunities that strengthen human decision-making.
- Prepare for adoption like it’s a product launch. Train users with real scenarios. Make it intuitive and transparent.
One of the most overlooked challenges isn’t the model accuracy; it’s frontline adoption. If your team doesn’t trust the AI or understand why it’s making a recommendation, it will simply be ignored, no matter how good it is.
CRM is no longer enough on its own
CRM remains an important tool in the healthcare IT ecosystem, but it’s no longer sufficient on its own. Patients expect personalization, speed and transparency. Providers and support teams need insights, not just dashboards. Regulators demand explainability and fairness. And the pace of change won’t slow down.
Looking ahead, CIOs will need to think beyond platforms and start designing AI-driven ecosystems where CRM is just one component. The next generation of patient experience will be shaped by how well we can bring together data, workflows and intelligence across the entire enterprise. That means investing not only in technology but also in the governance, culture and partnerships that allow AI to scale responsibly.
The opportunity is massive, but so is the responsibility. As digital leaders, we’re not just building systems, we’re shaping how patients experience care. And in that world, CRM is no longer the cockpit; it’s just one of many sensors feeding the AI-driven flight. The true pilot will be the CIOs and healthcare and tech leaders who can align innovation with trust, ethics and human impact.
This article is published as part of the Foundry Expert Contributor Network.
Want to join?